The War on Drugs is causing human rights violations on a global scale.
All over the world, people are subjected to police mistreatment, harassment and arbitrarily arrest simply for their choice of intoxicant. Many are subject to involuntary "treatment", which amounts to little more than prison labor camps. The "patients" (inmates) are either unpaid, or paid below the minimum wage and then nickel-and-dimed with administrative fees. Resistance is met with savage beatings, torture, sexual abuse and increased time added to their "rehabilitation". Most "patients" are forced into treatment without judicial overview or opportunity for appeal. Drug treatment, when present at all, is not evidence-based. (One example includes having the "patients" chant "Healthy!Healthy!Healthy!").
One product of these labor camps is shelled cashews and the US is an importer. If you buy shelled cashews in the US it is quite possible they were shelled by a fellow opiate user enslaved by the state. As part of their "treatment", the drug users are given quotas to fill. Failure to meet the quotas are met with severe punishment.
Opiophobia and the war on drugs is also the driving force behind the inhumane treatment of pain. Third world countries are especially hard hit, the supply does not come anywhere near the levels necessary to meet the demand. This is inexcusable, morphine is cheap and easy to produce. It is also remarkably safe when used properly. There is no maximum dose. It is also relatively safe, if one was to accidentally take double the expected dose, death or organic damage would be very unlikely. Whereas if one was on the highest recommended daily dosage of acetaminophen, and accidentally doubled the dosage serious liver damage may result. Addiction in patients taking opiates for pain is actually uncommon. Even young children and terminal patients are not excepted from their torments. And really, even if aggressive treatment with opiates did result in addiction, does it really matter when the person is dying? Is the risk of addiction sufficient to justify forcing someone to live in agony?
Criminalizing drug use itself undermines our basic human right to
autonomy and privacy, according to Human Rights Watch. I would also add
that it violates our freedom of medicine, and the right to self-medicate.
Since the US incarcerates more of its citizens than any other country in
the world, largely for drug "crimes", the US itself is one of the
world's greatest human rights violators. Government intransigence on the issue of harm reduction is causing an epidemic of HIV and hepatitis infections among injection drugs users, violating their right to a high standard of health.
From Human Right's Watch
(Antigua) – National drug control policies that impose criminal penalties for personal drug use undermine basic human rights, Human Rights Watch said today. To deter harmful drug use, governments should rely instead on non-penal regulatory and public health policies. The 43rd General Assembly of the Organization of American States, taking place in Antigua, Guatemala from June 4 to 6, 2013, will focus on drug control policy in the Americas.
Governments should also take steps to reduce the human rights costs of current drug production and distribution policies, Human Rights Watch said. Among the steps should be reforming law enforcement practices and exploring alternatives for legal regulation that would reduce the power of violent criminal groups.
[...]
Subjecting people to criminal sanctions for the personal use of drugs, or for possession of drugs for personal use, infringes on their autonomy and right to privacy, Human Rights Watch said. The right to privacy is broadly recognized under international law, including in the International Covenant on Civil and Political Rights and the American Convention on Human Rights. Limitations on autonomy and privacy cannot be justified unless they meet the criteria for any restriction of a basic right, namely legitimate purpose, proportionality, necessity, and non-discrimination.
While protecting health is a legitimate government purpose, criminalizing drug use to protect people from harming themselves does not meet the criteria of necessity or proportionality. Governments have many non-penal options to reduce harm to people who use drugs, including offering substance abuse treatment and social support.
Human Rights Watch research around the world has found that the criminalization of drug use has undermined the right to health. Fear of criminal penalties deters people who use drugs from using health services and treatment, and increases their risk of violence, discrimination, and serious illness. Criminal prohibitions have also impeded the use of drugs for legitimate medical research, and have prevented patients from accessing drugs for palliative care and pain treatment.
“There are many steps that governments can and should take to deter, prevent and remedy the harmful use of drugs,” Vivanco said. “But they shouldn’t do it by punishing the people whose health they are trying to protect.”
Governments have a legitimate interest in protecting third parties from harm resulting from drug use, such as driving under the influence, Human Rights Watch said. They may impose, consistent with human rights, proportionate criminal penalties on behavior that occurs in conjunction with drug use if that behavior causes or seriously risks harm to others.
With respect to drug use by children, governments have obligations to take appropriate legislative, administrative, social, and educational measures to protect children from the illicit use of drugs. Governments should not impose criminal penalties on children for drug use or possession, Human Rights Watch said.
“When someone under the influence of drugs does something that could harm others, whether it’s driving a car or endangering a child through neglect, criminal sanctions may be entirely appropriate, just as they are when people use alcohol in a way that endangers others,” said Vivanco. “However, the penalty is not for drug use alone but for engaging in activity that could endanger others while under the influence of drugs.”
Americas: Decriminalize Personal Use of Drugs
The article goes on to discuss human rights violations caused by the production and distribution of illicit drugs, and the reactionary role of the UN International Narcotics Control Board.
Below are specific reports from Human Rights Watch. I have grouped them into three categories: pain medicine access, abuse in the name of drug treatment, and general policy and HIV response.
Pain Treatment and Access to Medicine
Global State of Pain Treatment Access to Medicines and Palliative Care. June 3, 2011
This
128-page report details the failure of many governments to take even
basic steps to ensure that people with severe pain due to cancer, HIV,
and other serious illnesses have access to palliative care, a health
service that seeks to improve quality of life. As a result, millions of
patients live and die in great agony that could easily be prevented,
Human Rights Watch said.
“Please, do not make us suffer any more…” Access to Pain Treatment as a Human Right. March 3, 2009
In
this 47-page report Human Rights Watch said that countries could
significantly improve access to pain medications by addressing the
causes of their poor availability. These often include the failure to
put in place functioning supply and distribution systems; absence of
government policies to ensure their availability; insufficient
instruction for healthcare workers; excessively strict drug-control
regulations; and fear of legal sanctions among healthcare workers.
Human Rights Abuses in the Name of Treatment
Torture in the Name of Treatment Human Rights Abuses in Vietnam, China, Cambodia, and Lao PDR. July 24, 2012
More than 350,000 people identified as drug users are held in compulsory drug "treatment" centers in China and Southeast Asia. Detainees are held without due process for periods of months or years and may be subjected to physical and sexual abuse, torture, and forced labor. International donors and UN agencies have supported and funded drug detention centers, while centers have systematically denied detainees access to evidence-based drug dependency treatment and HIV prevention services. "Torture in the Name of Treatment," summarizes Human Rights Watch’s findings over five years of research in China, Cambodia, Vietnam, and Lao PDR.
“Skin on the Cable” The Illegal Arrest, Arbitrary Detention and Torture of People Who Use Drugs in Cambodia. January 25, 2010
In this 93-page report Human Rights Watch documents detainees being beaten, raped, forced to donate blood, and subjected to painful physical punishments such as "rolling like a barrel" and being chained while standing in the sun. Human Rights Watch also reported that a large number of detainees told of receiving rotten or insect-ridden food and symptoms of diseases consistent with nutritional deficiencies.
“Where Darkness Knows No Limits” Incarceration, Ill-Treatment and Forced Labor as Drug Rehabilitation in China. January 7, 2010
This 37-page report based on research in Yunnan and Guangxi provinces, documents how China's June 2008 Anti-Drug Law compounds the health risks of suspected illicit drug users by allowing government officials and security forces to incarcerate them for up to six years. The incarceration is without trial or judicial oversight. The law fails to clearly define mechanisms for legal appeals or the reporting of abusive conduct, and does not ensure evidence-based drug dependency treatment.
The Rehab Archipelago Forced Labor and Other Abuses in Drug Detention Centers in Southern Vietnam. September 7, 2011
The
121-page report documents the experiences of people confined to 14
detention centers under the authority of the Ho Chi Minh City
government. Refusing to work, or violating center rules, results in
punishment that in some cases is torture. Quynh Luu, a former detainee
who was caught trying to escape from one center, described his
punishment: "First they beat my legs so that I couldn't run off again...
[Then] they shocked me with an electric baton [and] kept me in the
punishment room for a month."
Somsanga’s Secrets Arbitrary Detention, Physical Abuse, and Suicide inside a Lao Drug Detention Center. October 11, 2011
This
report examines conditions in the Somsanga Treatment and Rehabilitation
Center, which has received a decade of international support from the
United States, the United Nations, and other donors. Detainees are held
without due process, and many are locked in cells inside barbed wire
compounds. Former detainees told Human Rights Watch that they had been
held for periods of three months to more than a year. Police and guards
are a constant presence, and those who try to escape may be brutally
beaten.
An Unbreakable Cycle Drug Dependency Treatment, Mandatory Confinement, and HIV/AIDS in China’s Guangxi Province December 9, 2008
In
China, illicit drug use is an administrative offense and Chinese law
dictates that drug users “must be rehabilitated.” In reality, police
raids on drug users often drive them underground, away from methadone
clinics, needle exchange sites, and other proven HIV prevention
services. And every year Chinese police send tens of thousands of drug
users to mandatory drug treatment centers, often for years, without
trial or due process.
This report finds that most mandatory treatment
centers, while ostensibly meant to provide drug treatment, do not
actually offer forms of drug dependence treatment internationally
recognized as effective. Mostly, drug users are forced to work or to
spend their days in crowded cells little different from prisons.
Barred from Treatment Punishment of Drug Users in New York State Prisons. March 24, 2009
In
this 53-page report, Human Rights Watch found that New York prison
officials sentenced inmates to a collective total of 2,516 years in
disciplinary segregation from 2005 to 2007 for drug-related charges. At
the same time, inmates seeking drug treatment face major delays because
treatment programs are filled to capacity. When sentenced to
segregation, known as "the box," inmates are not allowed to get or
continue to receive treatment. Conditions in the box are harsh, with
prisoners locked down 23 hours a day and contact with the outside
through visitors, packages, and telephone calls severely restricted.
Public Policy and HIV
Rehabilitation Required Russia’s Human Rights Obligation to Provide Evidence-based Drug Dependence Treatment. November 8, 2007
In this 110-page study, Human Rights Watch found that the treatment offered at state drug treatment clinics in Russia was so poor as to constitute a violation of the right to health. The report concluded that drug dependent people in Russia who want to overcome their dependence are left virtually to their own devices in their battle with this serious and chronic disease.
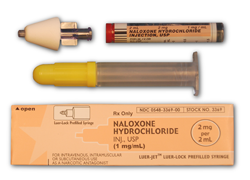
Injecting Reason Human Rights and HIV Prevention for Injection Drug Users. September 9, 2003
Government interference with sterile syringe programs is thwarting HIV prevention efforts in California. State laws and local enforcement are preventing drug users from obtaining the sterile syringes they need to protect themselves from HIV. This 61-page report documents police stopping, arresting, and harassing participants in needle exchange programs established by some California counties under state law. Even where needle exchange programs are legal, police remain authorized to arrest program participants under an antiquated law prohibiting the possession of “drug paraphernalia.” Over a quarter of new AIDS cases in the United States can be traced to infected syringes. Sharing syringes is also a major risk factor in the spread of hepatitis B and C. California is home to nearly one eighth of reported AIDS cases in the United States. The Human Rights Watch report recommends legalization of needle exchange programs and nonprescription pharmacy sales of syringes. It also calls on police departments to cease stops and seizures of participants in clean needle programs, a practice courts have recently prohibited in Connecticut, Massachusetts and New York.
Not Enough Graves The War on Drugs, HIV/AIDS, and Violations of Human Rights. July 8, 2004
This 60-page report provides fresh evidence of extrajudicial killings, arbitrary arrests and other human rights violations by Thai authorities. The report contains first-hand testimony from relatives of people killed during the drug war, as well as drug users who endured beatings, forced confessions and arbitrary arrests at the hands of Royal Thai Police. The government's anti-drug campaign has resulted in as many as 3,000 killings and has driven drug users underground and away from lifesaving HIV prevention services.
Abusing the User: Police Misconduct, Harm Reduction and HIV/AIDS in Vancouver. May 7, 2003
An anti-drug crackdown by the Vancouver Police Department has driven injection drug users away from life-saving HIV prevention services, raising fears of a new wave of HIV transmission in the city that is already home to the worst AIDS crisis in the developed world, said Human Rights Watch. In a 25-page report released today, “Abusing the User: Police Misconduct, Harm Reduction and HIV/AIDS in Vancouver,” Human Rights Watch documents instances of unnecessary force and mistreatment, arbitrary arrest, and other intimidation and harassment of drug users as part of a campaign commonly referred to as Operation Torpedo. The crackdown began on April 7 in the city’s impoverished Downtown Eastside neighborhood. Though drug traffickers are the ostensible target, drug users not charged with selling drugs have been driven to places where health workers cannot reach them to ensure access to sterile syringes and other HIV prevention services.
Courage in the Face of Death: The Thai Drug Users’ Network. July 13, 2004
Thailand
enjoys an international reputation as a “best practice” model in the
fight against AIDS principally because of its “100 percent condom”
campaign in the 1990s. This campaign engaged sex workers with the clear
recognition that they were part of the solution to a growing AIDS
epidemic. Drug users have not enjoyed the same recognition in Thailand.